This website is under construction. Please visit after a week for the complete website experience.
Paediatric Surgery, Shaikh Zayed Hospital, Lahore

Cervical Lymphadenopathy
Contents
-
Clinical Evaluation
-
Management Algorithm
-
What Next?
-
References
-
Examination Video
Basic Anatomy

The neck is divided broadly into an anterior triangle and a posterior triangle, separated by the sternocleidomastoid muscle. The anterior triangle (front) contains vital vessels (carotid artery, jugular vein) and nerves, divided into submental, submandibular, carotid, and muscular triangles. The posterior triangle (back) holds the brachial plexus and spinal accessory nerve, divided by the omohyoid muscle into occipital and supraclavicular (subclavian) triangles, crucial for understanding neck surgery and pathology.
Lymphatic fluid consists of an ultrafiltrate of blood collected within lymphatic channels which run throughout the entire body. The fluid is slow moving and transported from the head and extremities to the larger vessels which then drain into the venous system.
The numbered diagram on the right has the following labels:
1. Mandible
2. Stylohyoid muscle
3. Posterior belly of digastric
4. Anterior belly of digastric
5. Submandibular triangle
6. Submental triangle
7. Carotid Triangle
8. Sternocleidomastoid muscle
9. Occipital (Posterior) triangle
10. Superior belly of omohyoid
11. Muscular Triangle
12. Trapezius
13. Inferior belly of omohyoid
14. Supraclavicular (posterior) triangle
Key Contents of the triangles
The carotid triangle is bounded by the posterior belly of the digastric muscle and the superior belly of the omohyoid muscle. It contains the following structures:
-
Common Carotid Artery
-
Internal Carotid Artery
-
External Carotid Artery and its first five branches
-
Ascending pharyngeal artery
-
Superior thyroid artery
-
lingual artery
-
Facial artery
-
Occipital artery
-
-
Carotid sinus and carotid body
-
Internal Jugular Vein
-
Last three cranial nerves
-
Vagus Nerve
-
Spinal Accessory Nerve
-
Hypoglossal nerve
-
-
Ansa Cervicalis [?]
-
Cervical part of Sympathetic Chain
-
Carotid Sheath
-
Deep Cervical Lymph nodes

The submandibular triangle (or digastric triangle) is a key anatomical region in the neck, located below the jaw (mandible) and important for containing the submandibular salivary gland, lymph nodes, facial artery/vein, and nerves. It's defined by the mandible as its base and the anterior/posterior bellies of the digastric muscle as its sides, with a floor of mylohyoid and hyoglossus muscles, crucial for surgery and understanding infection spread from teeth.
The muscular triangle of the neck contains vital infrahyoid (strap) muscles like the sternohyoid, sternothyroid, and thyrohyoid, along with the thyroid and parathyroid glands, larynx, trachea, and esophagus.
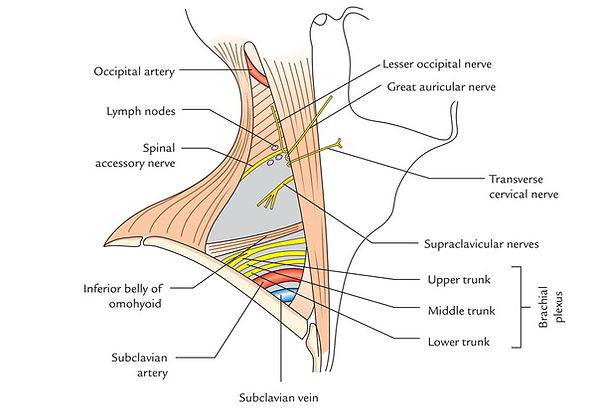
The posterior triangle of the neck contains vital nerves (brachial plexus, spinal accessory nerve, cervical plexus branches), major vessels, lymph nodes, and specific muscles (scalenes, levator scapulae, splenius capitis, omohyoid), divided by the omohyoid muscle into occipital and supraclavicular triangles
Lymph Node Levels
Cervical lymph nodes are organized into six standard surgical levels (I–VI) based on anatomical boundaries defined by muscles, bones, and blood vessels. This classification is used to predict the spread of head and neck cancers and to guide surgical dissections.
-
Level I: Submental & Submandibular
-
Level IA (Submental): Located between the anterior bellies of the digastric muscles; drains the chin and tip of the tongue.
-
Level IB (Submandibular): Found between the mandible and the digastric muscles; drains the oral cavity and submandibular gland.
-
-
Level II: Upper Jugular
-
Located along the upper third of the internal jugular vein (IJV), extending from the skull base to the hyoid bone.
-
Subdivided into IIA (anterior to the spinal accessory nerve) and IIB (posterior to the nerve).
-
-
Level III: Middle Jugular
-
Extends from the hyoid bone down to the cricoid cartilage along the middle third of the IJV.
-
-
Level IV: Lower Jugular
-
Extends from the cricoid cartilage down to the clavicle along the lower third of the IJV.
-
-
Level V: Posterior Triangle
-
Located behind the sternocleidomastoid muscle and in front of the trapezius.
-
Divided into VA (upper, above the cricoid level) and VB (lower, below the cricoid level).
-
-
Level VI: Anterior (Central) Compartment
-
Contains the pretracheal, paratracheal, and perithyroidal nodes around the thyroid and trachea.
-
Boundaries are the hyoid bone (superior), suprasternal notch (inferior), and common carotid arteries (lateral).
-
Additional Regions
-
Level VII: Superior mediastinal nodes, located below the suprasternal notch.
-
Non-Level Nodes: Important groups outside the standard six levels include the retropharyngeal, parotid, occipital, and retroauricular nodes.

Drainage Regions:
Face & Oropharynx: Preauricular, submandibular and submental and submental nodes
Posterior Scalp: Occipital Nodal Group
Mouth, Tongue, Superficial and deep chains of anterior cervical lymph nodes
tonsils, oropharynx,
nasopharynx:
Scrofula
Tuberculous cervical lymphadenitis, also known as scrofula is the most common manifestation of extrapulmonary tuberculosis and is a very frequent cause of a peripheral lymphadenitis in the developing world. Additionally, in industrialised nations, there is a resurgence among intravenous drug users (IVDU) and the immunocompromised population, especially those due to HIV.
Scrofula (tuberculous lymphadenitis) progresses through distinct stages:
Stage 1: Reactive Hyperplasia
Enlarged, firm, mobile lymph nodes with general inflammation, but not yet fixed.
Stage 2: Periadenitis
Nodes become large, rubbery, and fixed (stuck) to surrounding tissues due to inflammation (periadenitis).
Stage 3: Cold Abscess
Central softening occurs as the infection progresses, forming a "cold abscess" (lacking warmth, pus-filled).
Stage 4: Collar-Stud Abscess
The abscess develops a "collar-stud" shape, often appearing as two connected swellings, one deeper and one closer to the skin.
Stage 5: Sinus Tract Formation
The abscess ruptures through the skin, creating a persistent draining channel (sinus tract) that leaks pus and caseous material.

Lymphadenopathy
Lymphadenopathy is defined as an enlargement or a change in the character of a lymph node. Children have palpable nodes in most of the superficial lymphatic basins, including cervical, axillary, and inguinal regions that are non pathological; there is progressive increase in lymphoid mass from birth until early adolescence. This lymphoid tissue then normally diminishes throughout puberty.
Physiologically, cervical lymph nodes <2cm, axillary lymph nodes <1cm and inguinal lymph nodes < 1.5cm are non significant. Enlarged supratrochlear/epitrochlear [?], supraclavicular and popliteal (>0.5cm) lymph nodes are always pathological.
The differential diagnosis is as follows:

Classification
An effective classification of lymphadenopathy allows for accurate and expedient diagnosis and treatment. Lymphadenopathy can be classified as diffuse or solitary by anatomic location. Lymph nodes are organized in groups that drain specific regions of the body. This knowledge guides the clinician to inspect particular areas of anatomy when lymphadenopathy occurs. Specific anatomic regions include cervical (most common), salivary gland, breast, suboccipital, pre- or posterior auricular, submental, submandibular, mediastinal, axillary, inguinal, popliteal and supraclavicular (always pathologic).
Clinical Evaluation
History
A thorough history including the location, duration, progression and associated symptoms including pain, fever, weight loss and night sweats should be asked. Recent illnesses including upper respiratory tract infection, trauma, bites or dental problems should be evaluated.
A recent vaccination, especially BCG can cause transient lymphadenopathy. Other important points in history include recent travel, animal exposure and exposure to TB and tropical diseases.
Physical Examination
The area should be inspected for any colour change or visible marks over the swelling. On palpation, inspect whether the lymph node is solitary or multiple, matted or rubbery, smooth, soft or tender.
Infectious: Smooth, soft and tender
Neoplastic: Firm, fixed and non tender
-
Examination of skin and subcutaneous tissue that is drained by the affected lymph nodes should be evaluated. Examination of other lymph node basins should be performed.
-
Examination of thyroid for any thyroid nodule
-
Abdominal examination and search for organomegaly
Investigations
Laboratory Evaluation:
-
Complete Blood Count
-
Pancytopenia can be seen in leukemia
-
Lymphocytosis is seen with mononucleosis, cytomegalovirus.
-
-
ESR
-
C reactive protein
-
Tuberculin skin test
-
if history is suggestive of TB
-
-
Serum Lactate Dehydrogenase
-
if history is suggestive of lymphoma
-
-
Viral Serology
Radiological Evaluation
-
Chest radiograph (two view)
-
to rule out mediastinal masses that may compress the airway with or without significant symptoms
-
A chest radiograph should be performed prior to any operative intervention, including biopsies done under general anesthesia
-
Patients with large mediastinal masses compressing the airway should not undergo general anesthesia because this could result in airway collapse
-
-
Ultrasound with doppler






_edited.jpg)
_edited_edited.png)
_edited.jpg)